In the context of our Health Tech Guild, we are reviewing the main participants we design for. We consider this crucial to creating more human-centered products, and we’ve started with possibly the most relevant actor: The Clinician.
Clinicians are central figures in the healthcare ecosystem, balancing an overwhelming set of responsibilities ranging from patient care to dealing with complex administrative systems. As health technology continues to evolve, understanding how clinicians interact with these tools is critical for creating more effective solutions. This article explores the unique challenges clinicians face, especially regarding their relationship with technology and AI, and how designers and product developers can create tools that align with their real-world needs.
The Dual Role of Clinicians: Care and Administration
At their core, clinicians are driven by the goal of providing high-quality patient care. However, their daily routine is often overwhelmed by administrative tasks that compete for their attention. This tension between direct patient care and administrative work, such as managing electronic health records (EHRs) and coordinating with other healthcare providers, poses significant challenges. Clinicians often find themselves sacrificing patient interaction for paperwork, a trade-off that affects both their well-being and patient outcomes.
Clinicians’ struggles aren’t just personal issues—they directly impact the quality of care they provide. Designers need to recognize the weight of these responsibilities and ensure that health tech solutions streamline workflows, instead of adding new layers of complexity.

RELATED CHALLENGE:
How might we not just assist clinicians with administrative tasks but actively reduce them, so they can spend more time on patient care?
Relationships That Shape Healthcare
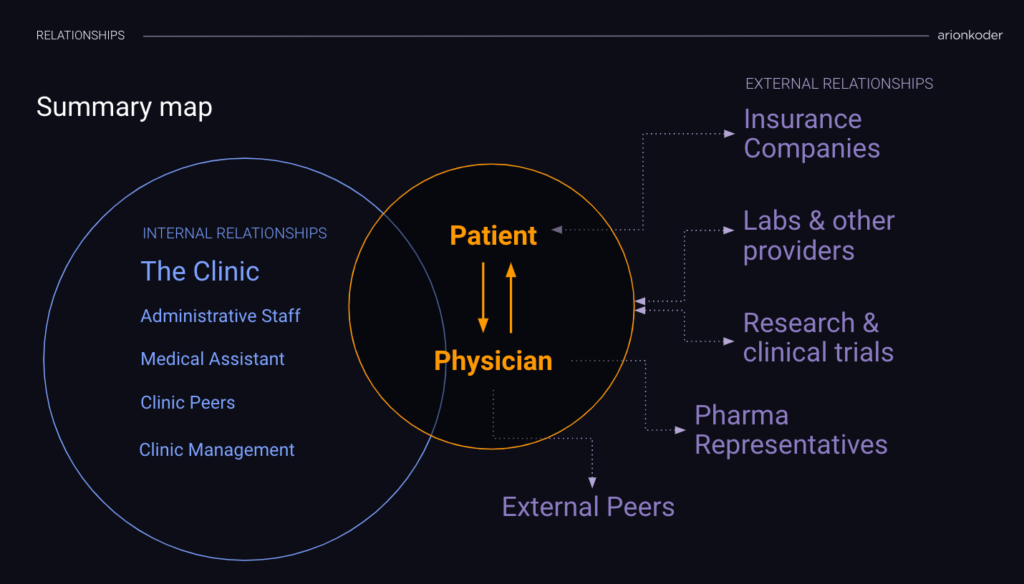
Clinicians operate within a complex web of internal and external relationships, each of which presents its own set of challenges. Internally, they collaborate with a diverse range of contributors, including administrative staff, medical assistants, and peers. However, coordinating within this network is often chaotic. Everyone is busy with their own workload, leaving little time for seamless communication or problem-solving. The fragmented nature of healthcare environments can result in missed information, delays, and a lack of clarity on patient status, which ultimately affects patient outcomes.
Externally, clinicians must navigate relationships with laboratories, pharmaceutical companies, insurance providers, and regulatory bodies. Sharing information with these entities is far from straightforward. Each entity may use different processes, technologies, or even formats, making it difficult for clinicians to coordinate care effectively. Moreover, concerns surrounding patient privacy further complicate the exchange of information, as clinicians must ensure compliance with strict healthcare regulations like HIPAA., which mandates the protection of sensitive patient data.
Health tech products must address these pain points by creating technology solutions that facilitate smoother collaboration, both internally and externally. Simplifying data sharing through interoperability, implementing strong privacy protections, and creating tools that allow busy healthcare professionals to coordinate without adding more burdens to their workflows should be central to any health tech solution.
RELATED CHALLENGE:
How might we break down the barriers caused by disparate systems, protect patient privacy, and still allow for smooth, efficient information sharing across the healthcare ecosystem?
The Tension Between Technology and Trust
When it comes to adopting new technologies, such as a new piece of software or an AI tool, clinicians often find themselves divided. This division starts with the clinician’s attitude. Some are enthusiastic about the potential of new technology while others are skeptical, wary of technology disrupting patient relationships or introducing new workflow challenges.
Beyond individual attitudes and resistance to change, the process of adopting new software is complex and multifaceted. Even if clinicians recommend a promising tool, clinic management and IT departments must review workflows and assess how the new technology integrates with existing systems. This process is delicate, as introducing a new system without considering its interaction with current processes can lead to disruptions in workflows, delays, or even patient safety risks. The integration process must also address learning curves for other clinic roles, such as nurses and administrative staff, who require time and training to adjust to the new system.
Additionally, security concerns play a significant role in the trust equation. Any new tool must meet stringent privacy and security standards, particularly in healthcare, where regulations such as HIPAA demand that patient data is carefully protected. IT teams need to evaluate potential vulnerabilities and implement robust protections to ensure sensitive data remains secure.
Focusing on AI as the latest technological disruption, despite its potential, trust remains a significant hurdle. Many clinicians are hesitant to rely on AI for critical decisions, particularly concerning accuracy, reliability, and ethical implications. As we mentioned in a previous article, this cautious approach is not only expected but also desirable. The challenge for designers lies in balancing the powerful capabilities of AI with the need for clinicians to feel in control of the decision-making process.
Health tech solutions that prioritize transparency, reliability, and clinician control are more likely to gain trust. By designing AI tools that act as decision-support systems rather than automated decision-makers, clinicians can harness the power of AI without feeling like they’re relinquishing control.
RELATED CHALLENGES:
- How might we create AI tools that enhance clinicians’ decision-making without diminishing their sense of control and responsibility
- How might we ensure seamless integration of new tools with minimal disruption to existing workflows and security frameworks?
Wrapping it up
Healthcare technology holds the power to redefine what is achievable in patient care. By addressing clinicians’ needs and the challenges they face in managing relationships, workloads, and new technologies, we can go beyond the expected and create tools that break new ground. The future isn’t just about making incremental improvements—it’s about reshaping the healthcare landscape, expanding the boundaries of what technology can do, and transforming clinicians’ ability to deliver the best care.
Human-centered design and AI play a crucial role in pushing these boundaries. However, this push for innovation brings inevitable tensions—between embracing the power of AI and maintaining the human-centered care that defines effective healthcare. By focusing on transparency, reliability, and clinician control, we can design AI tools that enhance decision-making without sacrificing the personal connection between clinicians and patients. Ultimately, AI should be seen as a supportive ally that empowers clinicians, not a disruptive force.
For health tech startups navigating these challenges—integrating new technologies, reducing administrative burdens, and ensuring seamless care coordination—our Reshape Health Grants offer a unique opportunity to enhance your AI-driven solutions. Learn more about how we support startups in this transformative journey at Reshape Health Grants 2024.
