In part one of this series on Building an AI-powered eligibility system for US healthcare, we explored the importance of understanding the problem domain and data before choosing AI implementation patterns. This article will deep dive into the solution process, the tools and frameworks we employed, and the challenges we encountered along the way.
Documenting the Solution: Tools for Technical Communication
Before diving into the architecture, the tools we used for documentation and diagramming are worth mentioning. Clear technical communication is crucial for complex projects and choosing the right visualization tools can make a significant difference.
For our documentation needs, we utilized two powerful and complementary tools:
1. Excalidraw (excalidraw.com)
- Used for high-level system overviews and conceptual diagrams
- Perfect for creating sketch-like, informal drawings that are easy to understand
- Collaborative features make it ideal for real-time design discussions
- We used it for our system overview diagram due to its ability to create friendly, approachable visualizations
2. Mermaid (mermaid.js.org)
- Used for more formal technical diagrams
- A code-based approach ensures consistency and version control
- Excellent for workflows, sequence diagrams, and database schemas
- We used it for detailed process flows and database relationships
Solution Overview
Our solution consists of three main components, each designed to handle specific aspects of the eligibility verification process:
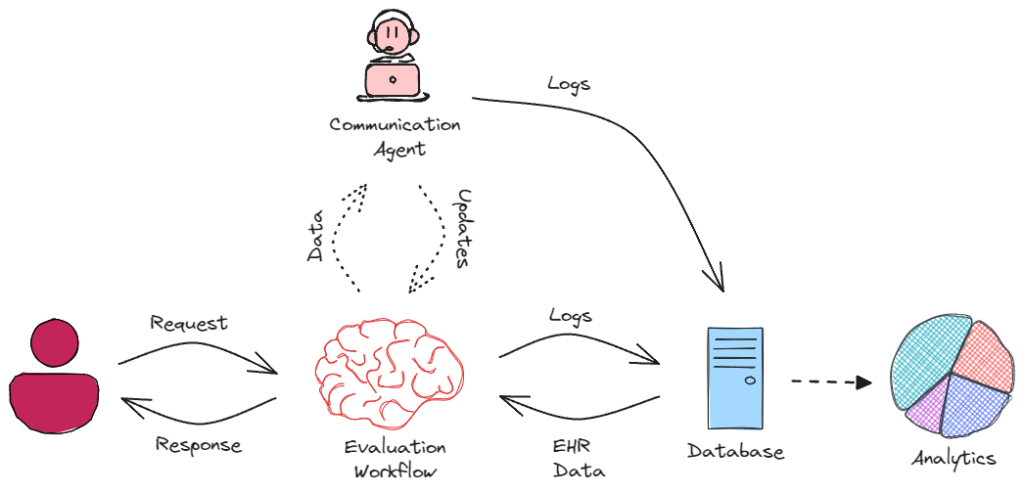
The high-level architecture shows the main components and their interactions:
- Communication Agent: Handles all user interactions
- Evaluation Workflow: Processes eligibility requests
- Database: Stores EHR data and interaction logs
- Analytics: Provides insights into system usage and outcomes
Communication Agent
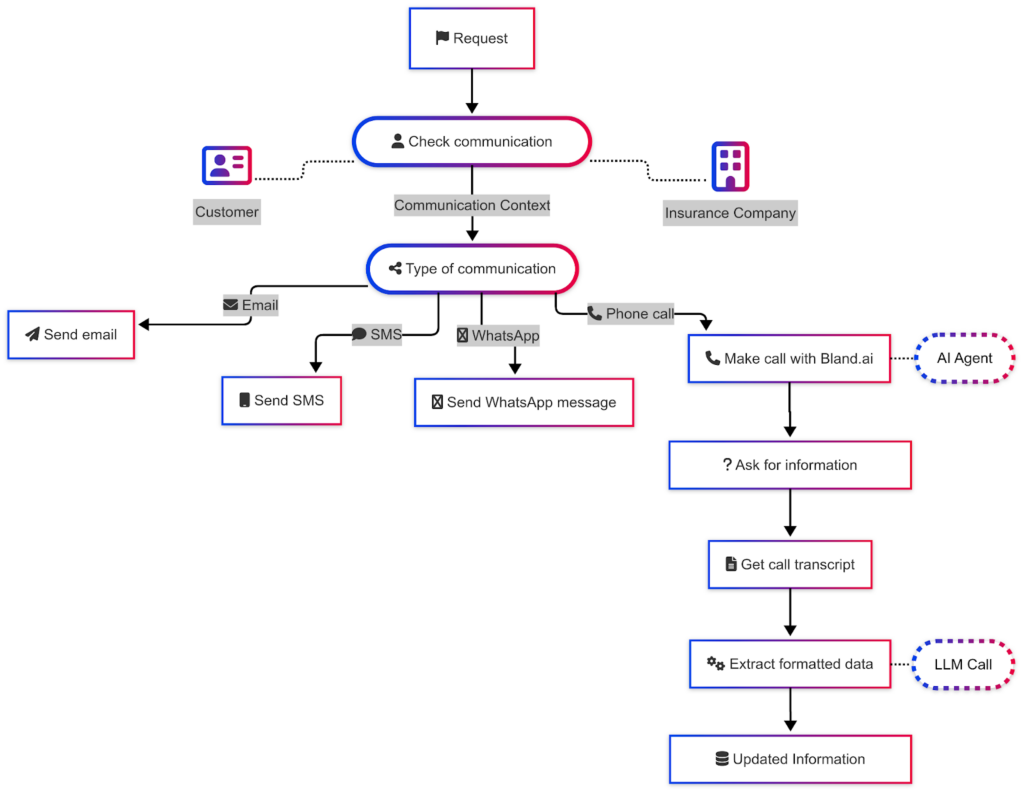
The Communication Agent system demonstrates our agent-based approach:
- Request handling and context determination
- Multi-channel support (Email, SMS, WhatsApp, Phone)
- AI Agent integration for voice calls using Bland.ai
- Data extraction and formatting using LLM
- Information management and updates
Evaluation Workflow
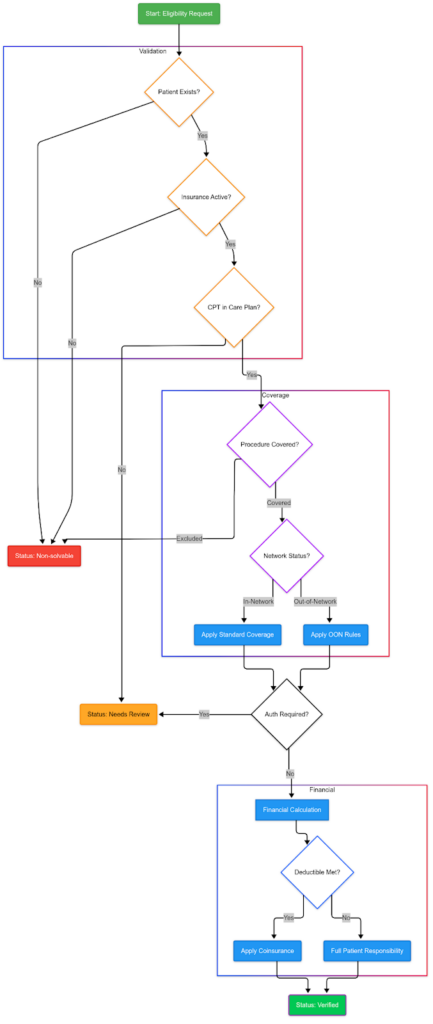
The Evaluation Workflow shows our structured approach to eligibility verification:
1. Validation Phase
- Patient existence verification
- Insurance status check
- CPT code validation
2. Coverage Assessment
- Procedure coverage verification
- Network status evaluation
- Application of standard or out-of-network rules
3. Financial Evaluation
- Deductible status check
- Cost-sharing calculation
- Final eligibility determination
Each component follows our established principles: using agents for flexible communication and workflows for structured processes. The system logs all interactions and decisions, enabling continuous improvement through analytics.
This architecture successfully balances the need for dynamic customer interaction with reliable, consistent eligibility determinations while maintaining the simplicity and transparency we aimed for in our design principles.
Lessons Learned in Building AI-Powered Healthcare Solutions
Our journey in developing an AI-powered eligibility verification system for healthcare revealed several crucial insights that can benefit similar projects in the future:
Start with Understanding, Not Technology
The sophistication of our AI tools didn’t determine the success of our implementation but our thorough understanding of the healthcare eligibility process. By starting with comprehensive data analysis and domain research, we built a foundation that informed all subsequent technical decisions.
Hybrid Approaches Work Best
Our dual-architecture approach – using an agent for communication and workflows for eligibility processing – demonstrated that different aspects of a complex system often require different solutions. The key is not to force a single architectural pattern across all components but to match the right tool to each challenge.
Data Structure Drives Success
The foundation of our system’s success lies in the meticulous design of the database schema, which was carefully crafted to reflect the complexities of real-world healthcare data. Leveraging Synthea’s synthetic healthcare dataset allowed us to simulate diverse patient scenarios, ensuring our schema could handle a wide range of use cases.
A well-structured data model not only streamlined workflow processing but also enhanced the reliability and maintainability of agent interactions. By organizing data into intuitive, normalized tables and establishing clear relationships between entities, we minimized redundancy and ensured data integrity. This robust structure enabled seamless integration with downstream processes, such as eligibility checks and reporting, while providing a solid foundation for future enhancements.
Balance Automation with Control
While AI-driven automation offers transformative potential, we recognized the importance of maintaining human oversight, especially in healthcare, where decisions can have life-altering consequences. Our workflow-based eligibility process strikes a careful balance: it harnesses AI’s efficiency and analytical power while embedding human review at critical junctures. This hybrid approach ensures consistent, auditable outcomes and mitigates the risks of over-reliance on automation. For example, AI algorithms pre-process and flag cases for review, but final decisions are made by trained professionals who can apply contextual judgment. This not only builds trust in the system but also ensures compliance with regulatory standards and ethical considerations.
Conclusion
This project demonstrates that successful AI implementation in healthcare hinges not on chasing technical novelty but on strategically aligning tools with well-understood human needs. By pairing the adaptability of conversational agents with the rigor of structured workflows, we’ve created a system that respects both the complexity of healthcare rules and the unpredictability of patient interactions. The most critical lesson—starting with domain understanding rather than technology—proved foundational, enabling simpler, more purposeful solutions.
As healthcare continues to evolve, this balanced approach offers a blueprint for responsible innovation: one that prioritizes patient outcomes over technical sophistication, maintains human accountability in automated systems, and proves that even in high-stakes environments, thoughtful AI integration can enhance operations without compromising safety or ethics.
Curious how AI agents can transform your business? Contact us and let’s start a conversation. We’re excited to share how we can help you navigate the future of AI.
